THE ULTRASOUND MOVEMENT- A CAREER RETROSPECTIVE
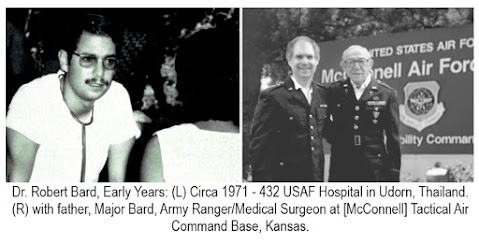
By: Dr. Robert Bard
I attribute my career in radiology to the US Air Force, having served in military hospitals in Thailand and Laos in the early ‘70’s. There, I witnessed the critical demands for immediate response and real-time diagnostic technology where time and accuracy are of the ultimate essence. I attribute my critical eye of many medical imaging devices to the 'battle hardened' challenges of a military hospital setting, easily paralleled to our emergency responders and the ICU facilities of today
Moving on to civilian life (back in the US), I watched diagnostic imaging history unfold throughout my career and marveled at the inspired evolution of the ultrasound protocol. Its remarkable growth in engineering, its data-gathering (quantifiable) milestones and breakthrough features conquered the arena of patient scanning while forging a safe, non-invasive and high-performance paradigm to physicians and health responders alike. From the high-powered large format hospital scanners to the latest in hand-held portable designs (aka. the digital stethoscope), ultrasound technology holds a solid place in the ever-shaping future of medicine and ancillary disciplines it supports. In 1974, my residency program director told me not to waste my time learning, ultrasound. I went to the Armed Forces Institute of Pathology in D.C. and then to Europe to advance my training. 50 years later, ultrasound has replaced many other invasive imaging technologies.
A GAME CHANGER IN PATIENT CARE
The point of care ultrasound unit practically reinvented the doctors' visit. By generating instantaneous scan results, the ultrasound completely supports the interactive collaboration between doctor & patient. Unlike any other scanning solution, the ultrasound is the only device that allows the patient to steer the probe to the exact area of pain or concern. The dynamics of its real-time output sets the stage for future tech designs.
In the United States, imaging is mostly performed by a technician where the patient holds no interactive part in the scanning process. In Europe, it is standard procedure for the medical team to perform the imaging directly on the patient - creating a more efficient diagnostic experience overall. Patient and physician can see what's going on and discuss treatment options at the same time. This real-time assessment comes direct from the doctor without any potential misinterpretation from secondary parties like the technician.
EARLY ADVANTAGES IN CANCER-SCANNING: AN HISTORICAL BOOST TO THE MAMMOGRAM
In 1976, during my early days as a young radiologist, I was approached by Dr. Henry Leis Jr., the pioneer doctor who wrote the very first text on breast cancer and developed mammography 18- a means of early diagnosis and instrumental in the use of many of the less invasive procedures used in the treatment of breast cancer today. He confessed with great concern that he had all these patients with lumpy or cystic breasts developing tumors that he could clearly feel but the mammogram kept missing it. Seeking my help through sonogram technology, we worked on his patients together and the sonogram clearly identified and quickly diagnosed a mass as either a cancer or a benign cyst, in a dense, lumpy breast. Since then we've incorporated the sonogram in high-risk patients’ regimen every six months religiously because it finds tumors while they're small and “lumpectomy” surgery is curative if the mass is less than 1 cm. This is alongside doing mammograms once a year in women over 50 or unless they have a history of cancer- at which case, we do it starting at age 45.
9/11 & DISASTER RESPONSE HEALTH ISSUES
A decade after the disaster, health reports continue to show thousands of new and aggressive cancer claims 15 years after the 9/11 attacks. By June, 2016, the Centers for Disease Control and the WTC Health Program enrolled more than 5,400 people who have been diagnosed with cancer within a two-year period (4,692 were first responders, recovery and cleanup workers and volunteers). Experts state that cancers from "burning asbestos and the entire toxic cauldron of Ground Zero" carries a latency period of 15-20 years after exposure, and a major spike in advanced cancer cases is expected within the next 10 years. With my practice centralized in midtown, Manhattan, first responders and civilians alike have received additional screening and monitoring for 9/11 related disorders as an alternative to standardized diagnostic protocols. The advantages of the 4D Doppler Technology helps to identify, detect and analyze many tumors from pre-malignant areas to advanced cancerous cases. The regular sonogram shows a malignant disorder while the 4D scan displays a mass filled with cancerous arteries and veins meaning this is highly aggressive requiring immediate attention.
INTERNATIONAL IMAGING ALLIANCE: UPGRADES FOR THE COVID FRONT LINES
2020- Thanks to its digital format, the ultrasound imaging protocol became the ideal medical collaboration platform, making electronic file sharing and remote/real-time scanning a complete reality. My international alliance comprised of research pioneers including
Dr. Danilo Buonsenso (Rome, Italy) who published reports about "ultrasound equipment as an effective replacement of the stethoscope.” Dr. Buonsenso's review presents the valid uses and benefits of Lung Ultrasound in identifying respiratory disorders that may be associated with Covid-19.
Front line physicians in Italy and Spain are reportedly triaging with portable (hand-held) ultrasound units that reduce logistical problems of a chaotic environment and healthcare worker exposure. Since imaging with CT or ultrasound is not diagnostic, determining who needs hospitalization is essential in a pandemic overwhelming medical providers. Dr. Buonsenso, at the viral epicenter in Rome, uses sonograms to decide who requires a CT scan. With the current pandemic, clinicians worldwide have been earmarking how identifying issues in the lungs (and the cardiopulmonary area) through the use of ultrasound equipment can be quite helpful in monitoring, screening, scanning and tracking pulmonary vulnerabilities and infections that may require follow-up testing for Coronavirus.
A SUSTAINABLE WORK PRACTICE
Burnout is a huge problem for the radiologic community. Imaging readers usually handle thousands upon thousands of images whereby interaction is only with a screen, not with the patient. Ultrasound scanning puts the radiologist in direct interactive contact with the patient each time. Here, the dynamics of patient care brings gratifying engagement in communicating diagnoses and CLOSURE with each patient's case. This work cycle is a significant upgrade in occupational endurance and consistent performance.