Today’s health conscious society means adults routinely seek reassurance about suspicious skin lesions. Diagnostic ultrasound examinations can accurately and rapidly differentiate between epidermal, dermal, and subcutaneous tissues in real time. This procedure may help to identify lesions invisible to the spatially restricted human eye. The high resolution and low cost of today’s ultrasonographic equipment allow this modality to be used readily in an outpatient office setting.
Today’s health conscious society means adults routinely seek reassurance about suspicious skin lesions. Diagnostic ultrasound examinations can accurately and rapidly differentiate between epidermal, dermal, and subcutaneous tissues in real time. This procedure may help to identify lesions invisible to the spatially restricted human eye. The high resolution and low cost of today’s ultrasonographic equipment allow this modality to be used readily in an outpatient office setting.The accuracy of ultrasonography in the epidermis, dermis, and subcutaneous tissues is both operator and equipment dependent. Standard 2-dimensional linear sonograms at 40 to 100 MHz image the epidermis. Probes using 15-to 22-MHz image the epidermis and dermis, including the adjacent tissues 1 to 2 cm deep to the basal dermal layer. Real time 3-dimensional (3D/4D) probes at 16 to 20 MHz using broadband technologies provide high resolution of these structures to a 4- to 7-cm depth in seconds. Today’s high-resolution equipment is a widely available imaging technology.
 MELANOMA
MELANOMAMalignant melanoma, one of the most lethal cancers, is increasing at an alarming rate. It is the leading cause of death in women aged 20-43 years. Importantly, only 1 out of 33,000 moles are malignant and sonography may prevent unnecessary biopsies. The chance of aggression is related to the tumor depth. Tumors less than 1 mm are often cured by biopsy. Disease greater in penetration is readily imaged by 3D Volumetric probes and non-palpable foci of tumor extension or lymph node (glands) involvement are visible in the scanned area. The metastatic potential is measured by the 3D Doppler study and follow up of distant tumor spread may be correlated with serial sonography. Some invasive surgical diagnostic procedures may be avoided by using high resolution imaging since scans detect tumor nests as small as 2 mm in the lymph nodes. This means that a sonogram guided needle biopsy may avoid the necessity of a massive radical operative dissection of otherwise healthy tissues.
DIAGNOSTIC APPLICATIONS FOR NON-MELANOMA SKIN CANCER: Clinical diagnosis is the primary modality used to identify nonmelanoma skin cancer; however, visual diagnosis alone cannot determine tumor depth. Imaging allows preoperative mapping of a lesion, which may alert the surgeon to the depth or subcutaneous extension of a lesion. This information allows surgical planning, which helps to limit the number of stages required and allow for preoperative planning to identify optimal techniques for surgical closure. The presence of coexisting benign disease, such as seborrheic hyperplasia or peritumor inflammatory reaction may falsely lead to a wider excision or inaccurate biopsy conclusions. Of basal cell carcinomas, 85% develop in the head and neck, showing a predilection for thin skin, such as the nose, lips, or eyelids. The various shaped probe constructions allow diagnostic evaluation of nearly all locations including external ear compartments (Fig. 2). Although most basal cell carcinomas lesions appear as well-defined, oval, echo-poor masses, lesions that may have a higher aggressive potential may also appear as hyperechoic spots.
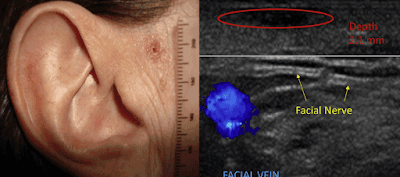
Fig. 1. Basal cell carcinoma echo-poor lesion (circle) 2.1 mm deep located 5 mm from the facial nerve (arrows) and 7 mm from temporal vein (blue).
 Fig. 2. Basal cell carcinoma (red circle) echo-poor mass in nasolabial groove imaged with small transducer to improve contact depth measurement of 1.5 mm.
Fig. 2. Basal cell carcinoma (red circle) echo-poor mass in nasolabial groove imaged with small transducer to improve contact depth measurement of 1.5 mm. Identification of these foci is useful because malignant neovascularity is less than that in other cancers. Indeed, the appearance of tortuous vessels suggests squamous cell carcinoma, Merkel cell carcinoma or metastatic tumor. The depth correlation between ultrasonography and histology is excellent, 5 which allows for better preoperative planning. (figure 3)
 Fig. 3. Basal cell carcinoma echo-poor mass with involvement of the orbicularis oculus muscle (m). Tumor (asterisk) echogenic foci signifies increased aggression and invades the dermis (d) and muscle layer (m) into the fat (arrow).
Fig. 3. Basal cell carcinoma echo-poor mass with involvement of the orbicularis oculus muscle (m). Tumor (asterisk) echogenic foci signifies increased aggression and invades the dermis (d) and muscle layer (m) into the fat (arrow).Squamous cell carcinoma presents as a hypoechoic lesion with irregular borders. Because the thickness or depth of invasion is an important predictor of metastases, the lesion should be followed along its entire course. Extra care is taken to find locoregional metastases and ultrasound examination of the liver and regional nodes may be performed simultaneously. The vascular pattern is increased diffusely throughout the entire mass as opposed to basal cell carcinomas, where the neovascularity is less prominent and often at the bottom of the lesion. Vascular mapping for major feeders with 3D ultrasonography is useful owing to the possibility of widespread penetration of the lesion.
TechReview: Exploring the DermaSensor™ - Until recently, the approach of identifying skin cancers was commonly a visual self-exam or a clinical exam conducted by a health care provider and/or a dermatologist. A skin biopsy is the only way to definitively diagnose skin cancer- where a small sample of the suspicious skin is removed and sent to a lab for examination (under a microscope) in search of cancer cells. HEALTHTECH REPORTER is proud to introduce another non-invasive advancement in skin cancer diagnostics. DermaSensor™ is an AI powered, FDA-cleared innovation designed to help physicians detect skin cancer at the point of care. According to a recent DEMO DAY @ Bard Diagnostics in NYC, clinical educators provided a comprehensive tour of what appears to be a ground-breaking innovation for primary care physicians "offering actionable results to aid in skin cancer detection by assessing cellular and sub-cellular features that cannot be seen visually or dermoscopically". DermaSensor™ was designed as a portable and fast-access noninvasive point-of-care assessment tool for primary care physicians to offer additional information about a lesion to aid in their consideration of a referral decision. (DermaSensor™ does not definitively determine whether or not cancer is present, specify what type of cancer may be present, or make any decision for the user.) |
HOW THE EXAMINATION IS PERFORMED: The application of ultrasonography depends on the area examined and equipment needed for specific diagnosis. All probes require gel contact with the skin and scan duration is typically proportional to the type of probe and examiner’s experience. Real-time imaging by a trained physician allows simultaneous picture generation and interpretation to occur within minutes. Routine 2D scan units require operator-dependent probe motion in 2 planes to obtain orthogonal images. The 3D imaging systems are operator independent because the probe is held steady over the area of interest and electronics scan a 4x4 cm area in 6 seconds. Patient motion rarely degrades the images owing to the rapid scan rate. Transducer size is matched to scan areas or can be focused to limited facial regions such as the nose. Three-dimensional imaging of ear and nose cartilage is also available with specialized probes. Lesions can be echogenic or hyperechoic (many internal echoes), such as hemorrhagic areas, echo poor or hypoechoic (few internal echoes), and echo free (no internal echoes), which are usually found in fluid, such as cysts.
ULTRASOUND EVALUATION OF DERMAL LESIONS: The incidence of melanoma and nonmelanoma skin cancer are both increasing. Earlier detection discovers smaller lesions where focal nonsurgical treatment may be preferred to standard operative techniques, which may limit potential long-term and postoperative side effects. Ultrasound examination permits rapid measurement of skin thickness, fat tissue depth, and fascial integrity. Medical imaging maps arteries, veins, and nerves providing preoperative landmarks reducing the risk of postoperative bleeding and nerve damage (Fig. 1). Image-guided treatment may also decrease the risk of postoperative disfigurement. Interval scans may also be used to track and assess lesions with low aggressive potential.
 About the Author:
About the Author:Robert L. Bard, MD, DABR, FAIUM, FASLMS is internationally known and recognized as a leader in the field of 21st Century 3-D ULTRASONOGRAPHIC VOLUMETRIC DOPPLER IMAGING. Dr. Bard specializes in advanced 3-D sonography to detect cancers in numerous organs including the breast, prostate, skin, thyroid, melanoma and other areas. Dr. Bard’s images are used to accurately guide biopsies, target therapy and provide focused follow-up after treatment.
As of Jan '18, Dr. Robert Bard spearheaded a partnership with a host of cancer educators, medical practitioners and non-profit foundations (allied under AwarenessforaCure.org) to form a public resource program to aid in the advancement of the public's understanding about self-preservation from cancer and other chronic diseases. EARLY DETECTION & PREVENTION is a global health movement that promotes a higher regard for "clean living" - from toxins and a toxic lifestyle. Our program consists of four main efforts: EDUCATION, COMMUNITY CONNECTION, CURRENT NEWS & CLINICAL RESOURCES. EARLY DETECTION & PREVENTION brings the empowerment of wellness through group seminars, videos and the distribution of current articles & newsletters published/shared to all the major cancer charities and their members.
For more information or to subscribe to our EARLY CANCER DETECTION & PREVENTION PROGRAM newsletter, contact Bard Cancer Diagnostics today at: 212.355.7017 (www.BardCancerDiagnostics.com)- or email us at: bardcancercenter1@gmail.com
Disclaimer & Copyright Notice: The materials provided on this website/web-based article are copyrighted and the intellectual property of the publishers/producers (The NY Cancer Resource Alliance/IntermediaWorx inc. and Bard Diagnostic Research & Educational Programs). It is provided publicly strictly for informational purposes within non-commercial use and not for purposes of resale, distribution, public display or performance. Unless otherwise indicated on this web based page, sharing, re-posting, re-publishing of this work is strictly prohibited without due permission from the publishers. Also, certain content may be licensed from third-parties. The licenses for some of this Content may contain additional terms. When such Content licenses contain additional terms, we will make these terms available to you on those pages (which his incorporated herein by reference).The publishers/producers of this site and its contents such as videos, graphics, text, and other materials published are not intended to be a substitute for professional medical advice, diagnosis, or treatment. For any questions you may have regarding a medical condition, please always seek the advice of your physician or a qualified health provider. Do not postpone or disregard any professional medical advice over something you may have seen or read on this website. If you think you may have a medical emergency, call your doctor or 9-1-1 immediately. This website does not support, endorse or recommend any specific products, tests, physicians, procedures, treatment opinions or other information that may be mentioned on this site. Referencing any content or information seen or published in this website or shared by other visitors of this website is solely at your own risk. The publishers/producers of this Internet web site reserves the right, at its sole discretion, to modify, disable access to, or discontinue, temporarily or permanently, all or any part of this Internet web site or any information contained thereon without liability or notice to you.