Saturday, July 26, 2025
Tuesday, July 15, 2025
Thursday, April 24, 2025
DR ROBERTA KLINE- SHOWCASE "ASK THE DOC"
Friday, April 18, 2025
Friday, March 21, 2025
Saturday, February 15, 2025
Wednesday, January 29, 2025
Monday, January 20, 2025
Sunday, January 12, 2025
Monday, December 30, 2024
Dr. Simpson on Imaging
I think imaging is extremely
important. And, you know, we talked about mentoring young people. Imaging is
not what you get when you don't know what's going on. I think imaging is there
to complement your physical examination and your thought process and to give
you the confidence that you're in the right area. If you look at burns, there
are very few experiences with imaging. There had been a laser doppler that was
looking at the second degree burns, showing you different colors, giving you a
sense of how deep that burn was, but the cost of that was just prohibitive. ,
and the question is when you use it, so if I'm gonna add something to burns in
the form of imaging. I'm gonna try to find out how much dermis is left on that
wound when I can't really see it in the beginning, follow it along to
understand that zone of injury, whether I'm losing the dermis, , and whether
it's an extremely deep burn because I wanna know whether I should treat that
patient a little more conservatively, with the expectation of healing.
, and that would be extremely
important. Third degree burn. , there's not much you can tell a very deep third
degree burn. If you look at the etiology, a flame burn, electrical burn, , that
tissue needs to be debrided. There's no question. But your second degree burns
your children where you're going to give them a little benefit of the doubt
because they have a different quality skin. If I had an imaging availability like ultrasound, which I think is easy to do. I
mean, you need the technical aspect, but if that can tell me as I saw in one of
his papers that I have a subdermal circulation still intact and that I have a
layer of dermis that's healthy, that would tell me I can go into skin
substitutes because this wound is going to heal. But you're going to need to
follow that up because a burn will change on a daily basis.
, you may get a sense that the
zone of injury is greater than you thought and you may be losing dermis in the
first two or three days. And that would lead us into stage two, which is not so
much can I get that burn to heal, but what is the quality of that healing
process? So if I have a very deep second degree burn and it takes two months
for that burn to heal, I'm not sure I've done, , a justice for that patient
because I know that the hypertrophic, restrictive scarring secondarily and even
the aesthetics of that burn secondarily, , may not be what I want. And it may
render the patient, , at a loss of function requiring more and more surgical
procedures to catch up when maybe I could have avoided that by entering early.
So imaging to show me the depth of the burn with consistency, follow that so I
can say, yes, I'll continue that skin substitute because this burn will heal
within two to three weeks, and I know that long term my scarring will be
acceptable.
And then the other thing I spoke with Dr. Bard about is looking at these burned scars after they've healed. And if you can image that and obtain a sense of quality of that scar, that would tell me whether therapy pressure treatment secondarily, will mature the scar enough so my function will return. If you look at the hand, a burn over the dorsal of the hand is going to be restrictive. If you can look at a patient who's been treated conservatively, but yet now there's hypertrophic scarring, can you tell me that that will mature with the right therapy and stretch? And if you can classify that or quantify that, then I would know whether I should intervene early because telling the patient, yes, you'll need three months of therapy, and by the way, you probably won't be much better than you were before. That's not what I want to see.
So this would give me early
insight into the quality of healing. So it's, will it heal and if it heals,
what is the quality? And I think those are the two major concerns that I have.
And I will tell you with skin substitutes, , I hear a lot, , I often at the
meetings would listen to the people at the tables and they would tell me what
they wanted to tell me, but I would often get access to the scientists behind
that and we would talk about those principles. So my question was, okay, you
can get this burn to heal, but if you're showing me something that heals in two
or three months, you know, talk to me about the quality of that healing
process. And that was usually something that I didn't hear very much about. So
that would be a great interest to me.
Awesome. , I'm gonna have a
part two to this question from my own self, , because we are constantly writing
about this term landmines, landmines, meaning surprises under the skin. Now
this isn't just on in terms of your field, but essentially there is a simpatico
between your expertise and dermatology in a sense that there's a lot of
different science, there's a lot of different areas to look at with skin if you
are working from skin down to be able to say that even we have, , a hair
implant, people with scalp for example, where before you start doing the
implants, do a quick scan of the scalp because there are landmines in there
that are possible. Well, we, we also call it lawsuit prevention, but we're not
publishing it in that term. Right? , , squamous cell melanoma carcinoma, these
things, believe it or not, show up underneath the skin and if you don't know
it, you could be popping something that that needs to be biopsied. Do you have
any thoughts in terms of using imaging to protect the clinician from surprises
or at least to be able to do a due diligence for the sake of safety for both
the clinician as well as the patient landmines?
Well, if, , if you're talking
about hair transplantation, , not something that I've really done very much of
in some burn cases, I've taken segments of skin with hair bearing tissue and
transferred those in. But I think imaging in that area would identify the
quality of the tissue in which you're putting that transplant into, has to be
well vascularized, the quality of softness. And if you can qualify that with
the imaging, I think you're ahead of that. , I think if you can show a
prophylactic process whereby you can look at these skin lesions and determine
are they squamous cell, , are they just keratosis in here? I mean, that would
be a tremendous asset for a dermatologist who has to biopsy a lot of these to
really get the answer they're looking for. So again, imaging would play a role,
, early on, allow you to follow it. , , imaging ultrasound, I imagine can be
reproducible very, very, very quickly, , and I imagine somewhat inexpensively.
And I think those are the keys to knowing what you're dealing with there. So
yeah, I think it plays a great role.
RESEARCH:
I think that would be something of interest to me. I mean, you know, I, I've been passionate about this for a very, very long time. A lot of it was in the surgical field, so you're operating all the time, but the thought process behind making the diagnosis, operating, getting the outcome you want, always something of been of interest to me. So yes, research I think is something I would be interested in.
Thursday, December 26, 2024
Wednesday, December 25, 2024
Wednesday, September 25, 2024
Video excerpts
LG Meets Living Beyond Breast Cancer (11/26)
Tuesday, September 17, 2024
Sunday, September 15, 2024
Friday, August 30, 2024
Friday, August 23, 2024
Tuesday, August 20, 2024
High-Frequency Ultrasound Examination of Melanoma and Skin Cancer
 Today’s health conscious society means adults routinely seek reassurance about suspicious skin lesions. Diagnostic ultrasound examinations can accurately and rapidly differentiate between epidermal, dermal, and subcutaneous tissues in real time. This procedure may help to identify lesions invisible to the spatially restricted human eye. The high resolution and low cost of today’s ultrasonographic equipment allow this modality to be used readily in an outpatient office setting.
Today’s health conscious society means adults routinely seek reassurance about suspicious skin lesions. Diagnostic ultrasound examinations can accurately and rapidly differentiate between epidermal, dermal, and subcutaneous tissues in real time. This procedure may help to identify lesions invisible to the spatially restricted human eye. The high resolution and low cost of today’s ultrasonographic equipment allow this modality to be used readily in an outpatient office setting.The accuracy of ultrasonography in the epidermis, dermis, and subcutaneous tissues is both operator and equipment dependent. Standard 2-dimensional linear sonograms at 40 to 100 MHz image the epidermis. Probes using 15-to 22-MHz image the epidermis and dermis, including the adjacent tissues 1 to 2 cm deep to the basal dermal layer. Real time 3-dimensional (3D/4D) probes at 16 to 20 MHz using broadband technologies provide high resolution of these structures to a 4- to 7-cm depth in seconds. Today’s high-resolution equipment is a widely available imaging technology.
 MELANOMA
MELANOMAMalignant melanoma, one of the most lethal cancers, is increasing at an alarming rate. It is the leading cause of death in women aged 20-43 years. Importantly, only 1 out of 33,000 moles are malignant and sonography may prevent unnecessary biopsies. The chance of aggression is related to the tumor depth. Tumors less than 1 mm are often cured by biopsy. Disease greater in penetration is readily imaged by 3D Volumetric probes and non-palpable foci of tumor extension or lymph node (glands) involvement are visible in the scanned area. The metastatic potential is measured by the 3D Doppler study and follow up of distant tumor spread may be correlated with serial sonography. Some invasive surgical diagnostic procedures may be avoided by using high resolution imaging since scans detect tumor nests as small as 2 mm in the lymph nodes. This means that a sonogram guided needle biopsy may avoid the necessity of a massive radical operative dissection of otherwise healthy tissues.
DIAGNOSTIC APPLICATIONS FOR NON-MELANOMA SKIN CANCER: Clinical diagnosis is the primary modality used to identify nonmelanoma skin cancer; however, visual diagnosis alone cannot determine tumor depth. Imaging allows preoperative mapping of a lesion, which may alert the surgeon to the depth or subcutaneous extension of a lesion. This information allows surgical planning, which helps to limit the number of stages required and allow for preoperative planning to identify optimal techniques for surgical closure. The presence of coexisting benign disease, such as seborrheic hyperplasia or peritumor inflammatory reaction may falsely lead to a wider excision or inaccurate biopsy conclusions. Of basal cell carcinomas, 85% develop in the head and neck, showing a predilection for thin skin, such as the nose, lips, or eyelids. The various shaped probe constructions allow diagnostic evaluation of nearly all locations including external ear compartments (Fig. 2). Although most basal cell carcinomas lesions appear as well-defined, oval, echo-poor masses, lesions that may have a higher aggressive potential may also appear as hyperechoic spots.
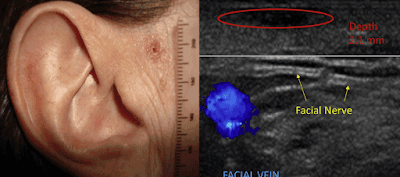
Fig. 1. Basal cell carcinoma echo-poor lesion (circle) 2.1 mm deep located 5 mm from the facial nerve (arrows) and 7 mm from temporal vein (blue).
 Fig. 2. Basal cell carcinoma (red circle) echo-poor mass in nasolabial groove imaged with small transducer to improve contact depth measurement of 1.5 mm.
Fig. 2. Basal cell carcinoma (red circle) echo-poor mass in nasolabial groove imaged with small transducer to improve contact depth measurement of 1.5 mm. Identification of these foci is useful because malignant neovascularity is less than that in other cancers. Indeed, the appearance of tortuous vessels suggests squamous cell carcinoma, Merkel cell carcinoma or metastatic tumor. The depth correlation between ultrasonography and histology is excellent, 5 which allows for better preoperative planning. (figure 3)
 Fig. 3. Basal cell carcinoma echo-poor mass with involvement of the orbicularis oculus muscle (m). Tumor (asterisk) echogenic foci signifies increased aggression and invades the dermis (d) and muscle layer (m) into the fat (arrow).
Fig. 3. Basal cell carcinoma echo-poor mass with involvement of the orbicularis oculus muscle (m). Tumor (asterisk) echogenic foci signifies increased aggression and invades the dermis (d) and muscle layer (m) into the fat (arrow).Squamous cell carcinoma presents as a hypoechoic lesion with irregular borders. Because the thickness or depth of invasion is an important predictor of metastases, the lesion should be followed along its entire course. Extra care is taken to find locoregional metastases and ultrasound examination of the liver and regional nodes may be performed simultaneously. The vascular pattern is increased diffusely throughout the entire mass as opposed to basal cell carcinomas, where the neovascularity is less prominent and often at the bottom of the lesion. Vascular mapping for major feeders with 3D ultrasonography is useful owing to the possibility of widespread penetration of the lesion.
TechReview: Exploring the DermaSensor™ - Until recently, the approach of identifying skin cancers was commonly a visual self-exam or a clinical exam conducted by a health care provider and/or a dermatologist. A skin biopsy is the only way to definitively diagnose skin cancer- where a small sample of the suspicious skin is removed and sent to a lab for examination (under a microscope) in search of cancer cells. HEALTHTECH REPORTER is proud to introduce another non-invasive advancement in skin cancer diagnostics. DermaSensor™ is an AI powered, FDA-cleared innovation designed to help physicians detect skin cancer at the point of care. According to a recent DEMO DAY @ Bard Diagnostics in NYC, clinical educators provided a comprehensive tour of what appears to be a ground-breaking innovation for primary care physicians "offering actionable results to aid in skin cancer detection by assessing cellular and sub-cellular features that cannot be seen visually or dermoscopically". DermaSensor™ was designed as a portable and fast-access noninvasive point-of-care assessment tool for primary care physicians to offer additional information about a lesion to aid in their consideration of a referral decision. (DermaSensor™ does not definitively determine whether or not cancer is present, specify what type of cancer may be present, or make any decision for the user.) |
HOW THE EXAMINATION IS PERFORMED: The application of ultrasonography depends on the area examined and equipment needed for specific diagnosis. All probes require gel contact with the skin and scan duration is typically proportional to the type of probe and examiner’s experience. Real-time imaging by a trained physician allows simultaneous picture generation and interpretation to occur within minutes. Routine 2D scan units require operator-dependent probe motion in 2 planes to obtain orthogonal images. The 3D imaging systems are operator independent because the probe is held steady over the area of interest and electronics scan a 4x4 cm area in 6 seconds. Patient motion rarely degrades the images owing to the rapid scan rate. Transducer size is matched to scan areas or can be focused to limited facial regions such as the nose. Three-dimensional imaging of ear and nose cartilage is also available with specialized probes. Lesions can be echogenic or hyperechoic (many internal echoes), such as hemorrhagic areas, echo poor or hypoechoic (few internal echoes), and echo free (no internal echoes), which are usually found in fluid, such as cysts.
ULTRASOUND EVALUATION OF DERMAL LESIONS: The incidence of melanoma and nonmelanoma skin cancer are both increasing. Earlier detection discovers smaller lesions where focal nonsurgical treatment may be preferred to standard operative techniques, which may limit potential long-term and postoperative side effects. Ultrasound examination permits rapid measurement of skin thickness, fat tissue depth, and fascial integrity. Medical imaging maps arteries, veins, and nerves providing preoperative landmarks reducing the risk of postoperative bleeding and nerve damage (Fig. 1). Image-guided treatment may also decrease the risk of postoperative disfigurement. Interval scans may also be used to track and assess lesions with low aggressive potential.
 About the Author:
About the Author:Robert L. Bard, MD, DABR, FAIUM, FASLMS is internationally known and recognized as a leader in the field of 21st Century 3-D ULTRASONOGRAPHIC VOLUMETRIC DOPPLER IMAGING. Dr. Bard specializes in advanced 3-D sonography to detect cancers in numerous organs including the breast, prostate, skin, thyroid, melanoma and other areas. Dr. Bard’s images are used to accurately guide biopsies, target therapy and provide focused follow-up after treatment.
As of Jan '18, Dr. Robert Bard spearheaded a partnership with a host of cancer educators, medical practitioners and non-profit foundations (allied under AwarenessforaCure.org) to form a public resource program to aid in the advancement of the public's understanding about self-preservation from cancer and other chronic diseases. EARLY DETECTION & PREVENTION is a global health movement that promotes a higher regard for "clean living" - from toxins and a toxic lifestyle. Our program consists of four main efforts: EDUCATION, COMMUNITY CONNECTION, CURRENT NEWS & CLINICAL RESOURCES. EARLY DETECTION & PREVENTION brings the empowerment of wellness through group seminars, videos and the distribution of current articles & newsletters published/shared to all the major cancer charities and their members.
For more information or to subscribe to our EARLY CANCER DETECTION & PREVENTION PROGRAM newsletter, contact Bard Cancer Diagnostics today at: 212.355.7017 (www.BardCancerDiagnostics.com)- or email us at: bardcancercenter1@gmail.com
Disclaimer & Copyright Notice: The materials provided on this website/web-based article are copyrighted and the intellectual property of the publishers/producers (The NY Cancer Resource Alliance/IntermediaWorx inc. and Bard Diagnostic Research & Educational Programs). It is provided publicly strictly for informational purposes within non-commercial use and not for purposes of resale, distribution, public display or performance. Unless otherwise indicated on this web based page, sharing, re-posting, re-publishing of this work is strictly prohibited without due permission from the publishers. Also, certain content may be licensed from third-parties. The licenses for some of this Content may contain additional terms. When such Content licenses contain additional terms, we will make these terms available to you on those pages (which his incorporated herein by reference).The publishers/producers of this site and its contents such as videos, graphics, text, and other materials published are not intended to be a substitute for professional medical advice, diagnosis, or treatment. For any questions you may have regarding a medical condition, please always seek the advice of your physician or a qualified health provider. Do not postpone or disregard any professional medical advice over something you may have seen or read on this website. If you think you may have a medical emergency, call your doctor or 9-1-1 immediately. This website does not support, endorse or recommend any specific products, tests, physicians, procedures, treatment opinions or other information that may be mentioned on this site. Referencing any content or information seen or published in this website or shared by other visitors of this website is solely at your own risk. The publishers/producers of this Internet web site reserves the right, at its sole discretion, to modify, disable access to, or discontinue, temporarily or permanently, all or any part of this Internet web site or any information contained thereon without liability or notice to you.
Wednesday, July 31, 2024
Process Report 1: Dr. H. Blatman on the progress of the VSELs Laser Guided Procedure
KINESIOLOGICAL ANALYSIS: VSELs TREATMENT PROGRESS EXPLAINED
By: Matthew Einsohn, ND
This might seem like a small thing, but it's actually a big deal. When you're sitting, lifting your leg involves working against gravity, which is already challenging. But when you're lying down, it requires a whole different set of muscles and coordination. It means engaging not just the hip flexors but also the core and stabilizing muscles of the lower back and pelvis. This shows his overall muscle function and coordination have significantly improved.
Without the help of gravity, his core muscles have to work even harder to stabilize and support the movement. This improvement in core strength is great news. Plus, this movement indicates improved flexibility and range of motion, likely due to decreased muscle stiffness and better neuromuscular control.Being able to perform this movement both sitting and lying down means his nervous system and muscles are working together more effectively. This is crucial for overall mobility and daily activities.
When Dr. Blatman is discussing the origins of pain, which is associated with sheer force and pressure, it appears that stabilization has been achieved. Based on watching the video a couple times, I would theorize that significant restoration is occurring. It seems he has addressed the root cause of the pain by restoring the integrity of the fascia.
Additionally, while there is a notion that one can make injuries less noticeable, this approach does not seem to align with his method. Instead, if he is indeed focusing on restoring the integrity of the fascia, it suggests that he is addressing the fundamental issue underlying the pain rather than merely masking the symptoms.
Some conditions just this mechanism can help with:
* Muscle weakness and atrophy from post-stroke rehabilitation or muscle degenerative diseases
* Neurological disorders such as MS or Parkinson's
* Recovery from spinal injuries
* Any chronic pain such as Fibromyalgia
* Anyone with joint or mobility problems
Muscle Weakness and Atrophy: Conditions causing muscle weakness or atrophy, such as post-stroke rehabilitation or muscle degenerative diseases, might see improvements in strength and coordination with similar treatments.
Neurological Disorders: Disorders like multiple sclerosis or Parkinson's disease, where muscle control and coordination are affected, could benefit from enhanced muscle function and coordination.
Post-Surgical Rehabilitation: Recovery from surgeries, especially orthopedic or spinal surgeries, could be supported by treatments that improve muscle strength, flexibility, and functional movement.
Chronic Pain Conditions: Conditions like fibromyalgia or chronic back pain that involve muscular and structural issues might see relief through better muscle engagement and reduced stiffness.
Balance and Stability Issues: Treatments that enhance core strength and overall muscle coordination can help with balance and stability, which is crucial for individuals with vertigo or balance disorders.
Joint and Mobility Problems: For conditions like arthritis or other joint issues, improving range of motion and muscle strength can reduce pain and enhance mobility.
Sports Injuries: Athletes recovering from injuries might benefit from improved muscle function and coordination, aiding in a quicker and more effective recovery.
-
A SURGEON'S BEST PRE-OP PARTNER by: Dr. Robert Bard As health practitioners, we are so fortunate to be part of an era where inform...
-
Disclaimer: The information (including, but not limited to text, graphics, images and other material) contained in this article is for infor...
-
FOREWORD by Dr. Robert Bard The modern era of diagnostic clinical imaging continues to expand in areas of optimal speed, sensitivity and fe...